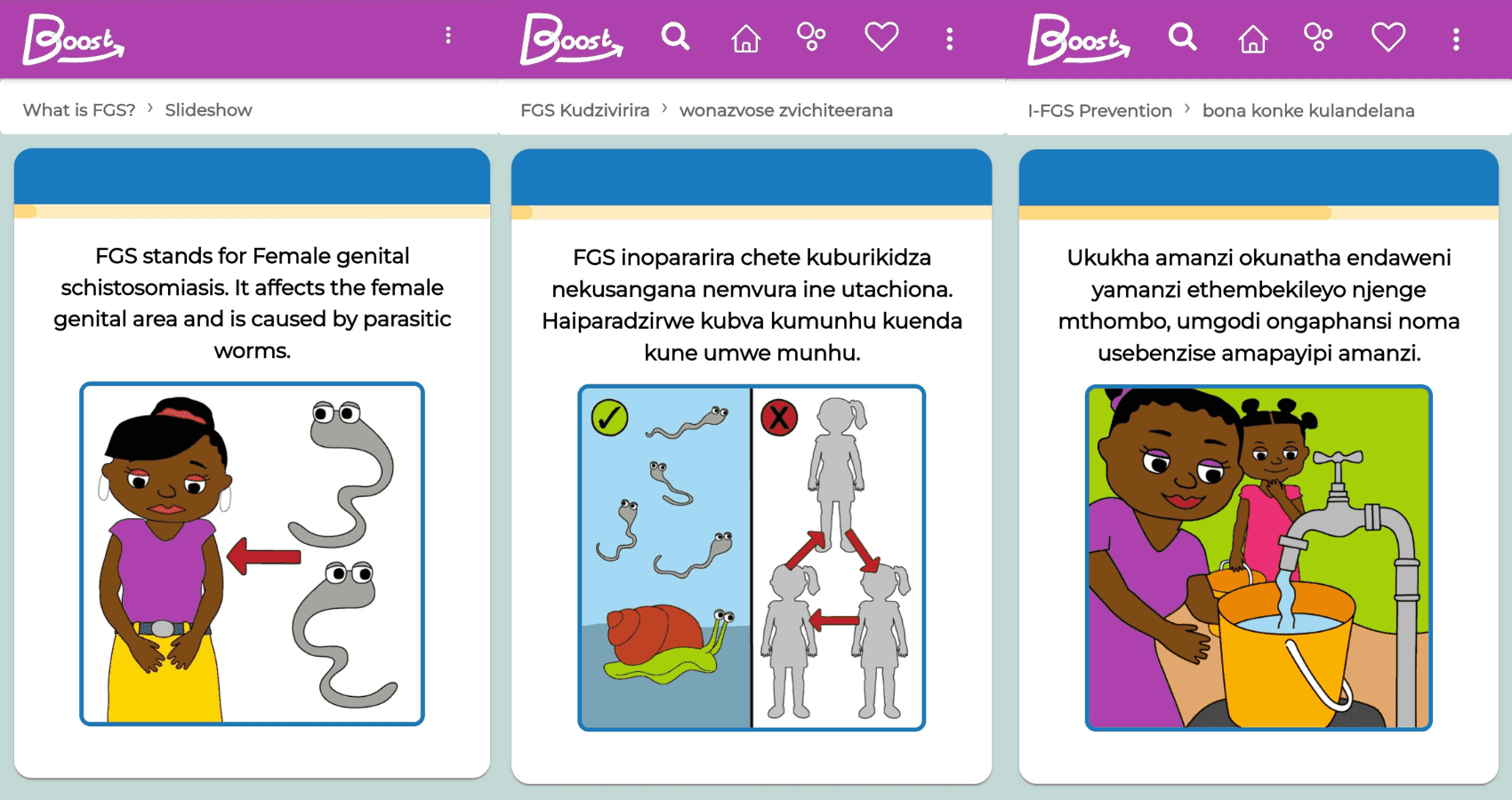
Schistosomiasis, also known as bilharzia or snail fever, is a neglected tropical disease (NTD) that is caused by tiny, parasitic, blood-dwelling worms that are found in freshwater lakes, ponds and rivers, primarily in countries across Africa. The tiny worm is not visible to the naked eye and enters a person's blood system without them knowing. This happens when they are using infected lakes, ponds and rivers for activities such as bathing, washing, collecting water and fishing. Schistosomiasis is a disease of poverty.
Female Genital Schistosomiasis (FGS) is when schistosomiasis affect the female genital area, causing inflammation, open sores and bleeding on the cervix and vagina.
Although both preventable and treatable, levels of FGS awareness, access to the drug Praziquantel and equipment are all limited. As a result, FGS is commonly misdiagnosed and treated as a sexually transmitted infection (STI) – leading to years of suffering and stigma for women living with the disease.
If left untreated FGS puts women at risk of serious reproductive health issues, including infertility and cervical cancer. FGS also makes women and girls more vulnerable to HIV due to the presence of sores which can bleed and provide an entry point for the virus. Some studies have found that women with FGS are 3-4 times more likely to also have HIV.
Given the high prevalence of HIV in many FGS endemic areas it is essential that a holistic client-centred approach is taken that recognises the interlinkages between these two conditions.